Assessing Patients with Symptoms
of Preterm Birth
Determining which patients are in preterm labor is a significant challenge. The majority of women who present with symptoms may not be at risk for preterm birth. In fact, many of these women ultimately deliver at term.1 However, the consequences of missing the opportunity to provide critical interventions in even one patient can be significant.
Standardizing care is critical to improving outcomes

SMFM recommends:2
“Even without new research, it may be possible to improve performance by simply encouraging clinicians to thoughtfully evaluate the actual risk of birth within 7 days before giving corticosteroids to patients whose risk may be fairly low, such as those with an asymptomatic short cervix, or those with contractions but a long, closed cervix and negative fetal fibronectin test result.”

AJOG states:3
“The failure to accurately predict impending preterm delivery was apparent from the Liggins and Howie study, in which approximately 1 in 3 women delivered >7 days after ACS administration. We have known for >50 years that timing is everything in regard to ACS efficacy, but the precision in our administration timing has not improved.
By 2019, only 15% to 40% of women treated with ACS were treated within the optimal window of 7 days before delivery, leading to an approximate 50% reduction in expected benefit, irrespective of confounders. It has been estimated that for every 3 to 4 cases of premature births in which ACS were administered >7 days before delivery, the associated increase in neonatal mortality (when compared with those cases in which ACS administration was optimally timed) is roughly equivalent to the neonatal mortality associated with 1 case of failure to administer ACS.”
ACOG recommends:4
“Protocols and checklists should be recognized as a guide to the management of a clinical situation or process of care that will apply to most patients.”
“Obstetrician-gynecologists should be engaged in the process of developing guidelines and presenting data to help foster stakeholder buy-in and create consensus, thus improving adherence to guidelines and protocols.”

ACNM recommends:5
“Evidence-based methods of identifying women at risk for premature labor, including ongoing risk assessment at each visit, screening women with preterm labor contractions using fetal fibronectin (fFN) testing, and screening using cervical length measurement techniques should be accessible in all practice settings.”

AWHONN recommends:6
“Structured systems may help to optimize communication about and response to rapid changes in patient status. There are a number of elective strategies that can be applied to maternity care:
- Communication tools such as Situation-Background-Assessment-Recommendation (SBAR)
- Training in principles of crew resource management
- Drills and simulations
- Debriefings and case reviews
- Organized board rounds, huddles, structured handoffs, and bedside rounds
- Checklists and standard order sets”
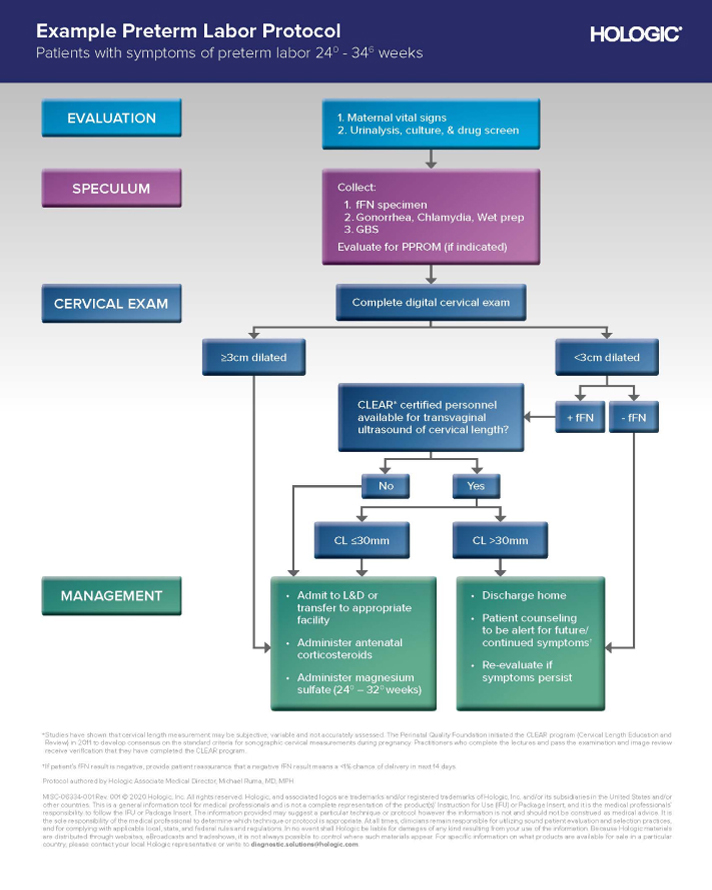
Improve outcomes with a standardized preterm labor triage protocol that begins with Rapid fFN sample collection
Rapid fFN testing is objective
Multiple studies have shown that clinical assessment alone cannot reliably rule out imminent preterm birth in patients presenting with symptoms of preterm labor.7 When combined with clinical assessment, fFN testing can help rule out imminent preterm birth with a 99.5% negative predictive value.1
Contractions alone cannot accurately assess a patient’s risk of imminent preterm birth.7
Cervical dilation alone cannot reliably assess a patient’s risk of imminent preterm birth.8
A real-world 20,000+ patient study shows that 20% of patients with symptoms of PTL, who were discharged home, went on to deliver within 72 hours.9
Cervical dilation alone cannot reliably assess a patient’s risk of imminent preterm birth.8
A real-world 20,000+ patient study shows that 20% of patients with symptoms of PTL, who were discharged home, went on to deliver within 72 hours.9
Rapid fFN testing is objective
Multiple studies have shown that clinical assessment alone cannot reliably rule out imminent preterm birth in patients presenting with symptoms of preterm labor.7 When combined with clinical assessment, fFN testing can help rule out imminent preterm birth with a 99.5% negative predictive value.1
Contractions alone cannot accurately assess a patient’s risk of imminent preterm birth.7
Cervical dilation alone cannot reliably assess a patient’s risk of imminent preterm birth.8
A real-world 20,000+ patient study shows that 20% of patients with symptoms of PTL, who were discharged home, went on to deliver within 72 hours.9
Contractions alone cannot accurately assess a patient’s risk of imminent preterm birth.7
Cervical dilation alone cannot reliably assess a patient’s risk of imminent preterm birth.8
A real-world 20,000+ patient study shows that 20% of patients with symptoms of PTL, who were discharged home, went on to deliver within 72 hours.9
fFN is a powerful tool that can be used alongside other diagnostic modalities
Adding fFN testing to cervical length can improve preterm birth prediction by as much as 50%.10
Assess preterm birth risk with the Rapid fFN test
Contact us for more information about Rapid fFN®.
Assess preterm birth risk with the Rapid fFN test
Contact us for more information about Rapid fFN® test.
1. Rapid fFN for the TLiIQ System [package insert]. AW-24196-001, Rev. 001, San Diego, CA: Hologic, Inc.; 2020 2. Society for Maternal-Fetal Medicine (SMFM)*; Rebecca Feldman Hamm, MD, MSCE; C. Andrew Combs, MD, PhD; Paola Aghajanian, MD; and Alexander M. Friedman, MD, MPH; Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine Special Statement: Quality metrics for optimal timing of antenatal corticosteroid administration, American Journal of Obstetrics and Gynecology (2022), doi: https://doi.org/10.1016/j.ajog.2022.02.021. 3. Vidaeff AC, Belfort MA, Kemp MW, et al. Updating the balance between benefits and harms of antenatal corticosteroids. American Journal of Obstetrics and Gynecology. 2022. doi:10.1016/j.ajog.2022.10.002 4. ACOG. Committee Opinion No. 629. Clinical Guidelines and Standardization of Practice to Improve Outcomes. Obstet Gynecol. 2015 Apr; 125(4):1027-9. 5. Division of Standards and Practice Clinical Standards and Documents Section; Approved by the ACNM Board of Directors: June 2012; www.midwife.org. 6. Association of Women’s Health, Obstetric, and Neonatal Nurses. Quality patient care in labor and delivery: a call to action. J Obstet Gynecol Neonatal Nurse. 2012;41:151-53. 7. Iams J, et al. Fetal fibronectin improves the accuracy of diagnosis of preterm labor. Am J Obstet Gynecol. 1995; 173(1):141-145. doi.10.1016/0002-9378(95)90182-5. 8. How H, et al. Cervical dilatation on presentation for preterm labor and subsequent preterm birth. Am J Perinatol. 2009;26;1-6. doi.10.1055/s-0028-1090586. 9. Blackwell SC, et al. Utilization of fetal fibronectin testing and pregnancy outcomes among women with symptoms of preterm labor. Clinicoecon Outcomes Res. 2017;9:585-594. 10. R Gomez, et al. Cervicovaginal fibronectin improves the prediction of preterm delivery based on sonographic cervical length in patients with preterm uterine contractions and intact membranes. Am J Obstet Gynecol. 2005; 192: 350-359