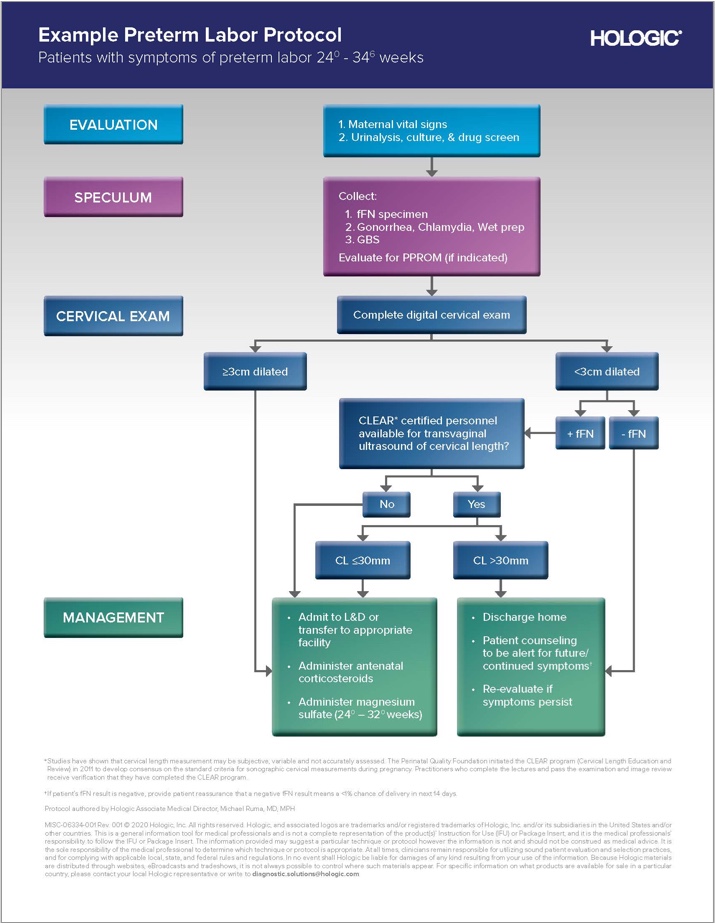
Assessing patients with symptoms of preterm labor
Determining which patients are in preterm labor is a significant challenge. The vast majority of women presenting with symptoms of preterm labor are not in true preterm labor and will go on to give birth at term.1 However, the consequences of missing the opportunity to provide critical interventions in even one patient can be significant.
Standardizing care is critical to improving outcomes



Clinical assessment alone is subjective and not predictive
Multiple studies have repeatedly shown that clinical assessment alone cannot reliably rule out imminent preterm birth in patients presenting with symptoms of preterm labor.5, 6 fFN testing has significantly better negative predictive values (NPV) and positive predictive values (PPV) than clinical assessment, plus the best sensitivity to help rule out preterm labor.1,5,7
Contractions are a poor way to assess if a patient is at risk of imminent preterm birth.5
Cervical dilation is a poor way to assess if a patient is at risk of imminent preterm birth.8
A real-world 20,000+ patient study shows that 20% of patients with symptoms of PTL, who were discharged home, went on to deliver within 72 hours.9
Adding fFN testing increases predictivity of cervical length6
Accurate results are variable even in the hands of skilled and well-trained clinicians when assessing risk of preterm birth by cervical length (CL). Adding fFN testing to cervical length can dramatically improve preterm birth prediction by as much as 50%.